Scientists are learning about the pros and cons of Ozempic in real-time, as prescriptions of the appetite-suppressing drug explode into the millions worldwide.
What started as a diabetes medication looks extra promising for heart health, even for those who don’t lose much weight, and now, experts are learning of the drug’s potential benefits to kidney health, too.
A large international trial, funded by the pharmaceutical supplier of Ozempic, Novo Nordisk, suggests that when the medication is given at a lower dose than is common for diabetes or weight loss, the kidneys seem to profit.
The trial involved more than 3,500 participants from 28 different countries with type 2 diabetes and chronic kidney disease – a combination of illnesses that puts individuals at a much higher risk of kidney failure and at-times fatal cardiovascular events, like heart attacks.
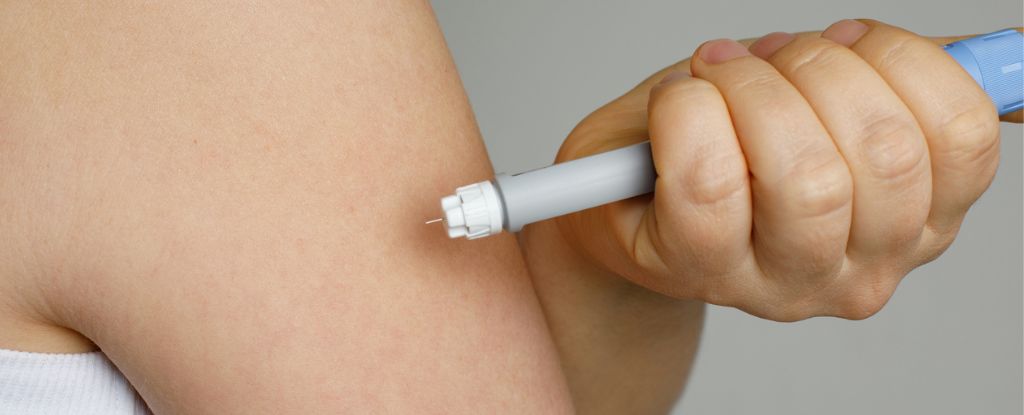
Between June 2019 and May 2021, half the participants in the trial randomly received a small weekly dose of semaglutide, the active ingredient in Ozempic. The other half received a placebo.
Those receiving the weekly injections showed a slower loss of kidney function, a reduced risk of kidney failure, lower systolic blood pressure, and reduced body weight compared to the placebo group.
After 3.4 years, participants on Ozempic experienced a 24 percent lower risk of major kidney events, an 18 percent lower risk of experiencing a heart attack or another major cardiovascular event, and a 20 percent lower risk of death from any cause.
“We would be saving kidneys, hearts, and lives in this population by making this drug available to them and that’s quite extraordinary for one treatment to be able to do,” says nephrologist Vlado Perkovic, from the University of New South Wales in Australia.
“One of the most common causes of kidney disease is diabetes, particularly type 2 diabetes, which has also been growing dramatically in recent decades.”
Obviously, Novo Nordisk has a financial incentive to find more ways to prescribe Ozempic, but the jump from diabetes treatment to kidney treatment isn’t such a big one.
Type 2 diabetes is the most frequent cause of chronic kidney disease in many nations, and other drugs that seek to balance blood glucose are already prescribed to protect the kidneys and reduce the risk of adverse cardiovascular outcomes in patients.
Initial studies, with and without industry funding, suggest that Ozempic could have benefits for the health of kidneys, which play a key role in removing waste and fluid in the body and controlling blood pressure.
Nevertheless, few trials have “recruited substantial numbers of participants with considerably reduced kidney function,” Perkovic and his colleagues write in their published paper.
“The cardiovascular and survival benefits of semaglutide in such patients are particularly important, since they are among the populations at highest risk for cardiovascular disease and death,” the team adds.
Semaglutide is classified as a glucagon-like peptide-1 (GLP-1) receptor agonist, meaning it mimics a natural hormone in the human body to improve blood sugar control and suppress appetite.
It’s not yet understood why semaglutide and other GLP-1 agonists on the market, such as liraglutide and tirzepatide, have positive effects on cardiovascular and kidney health.
While weight loss could be a contributing factor, recent studies on Ozempic suggest a reduction in body fat is likely only one of many processes involved.
Like heart cells, cells in the kidney display GLP-1 receptors, so researchers suspect that the protective effects of Ozempic seen in early evidence could be due, in part, to the drug acting directly on the kidneys, which may result in less inflammation and oxidative stress.
The medicine could also have indirect effects, such as lowering blood glucose levels, blood pressure, and body weight – all of which can alleviate pressure on the kidneys.
For now, however, these are just hypotheses. Further research is needed to understand how semaglutide and similar drugs actually impact the major organs of the body.
Given the limited treatment options available to those with diabetic kidney disease, current guidelines from both the American Diabetes Association and the Korean Diabetes Association recommend that clinicians consider prescribing GLP-1 receptor agonists.
Researchers now want to investigate whether this class of medication also works for chronic kidney disease in general, or if it is just useful for those with diabetic kidney disease specifically.
The study was published in the New England Journal of Medicine.










