In a new study published in Neuropsychopharmacology Reports, a team of scientists has shed light on the potential of delta opioid receptors to mitigate anxiety through the activation of a specific brain pathway. Their research unveils the intricate mechanisms by which the selective DOP agonist, KNT-127, reduces anxiety-like behavior in mice, marking a significant step towards developing novel treatments for anxiety-related disorders.
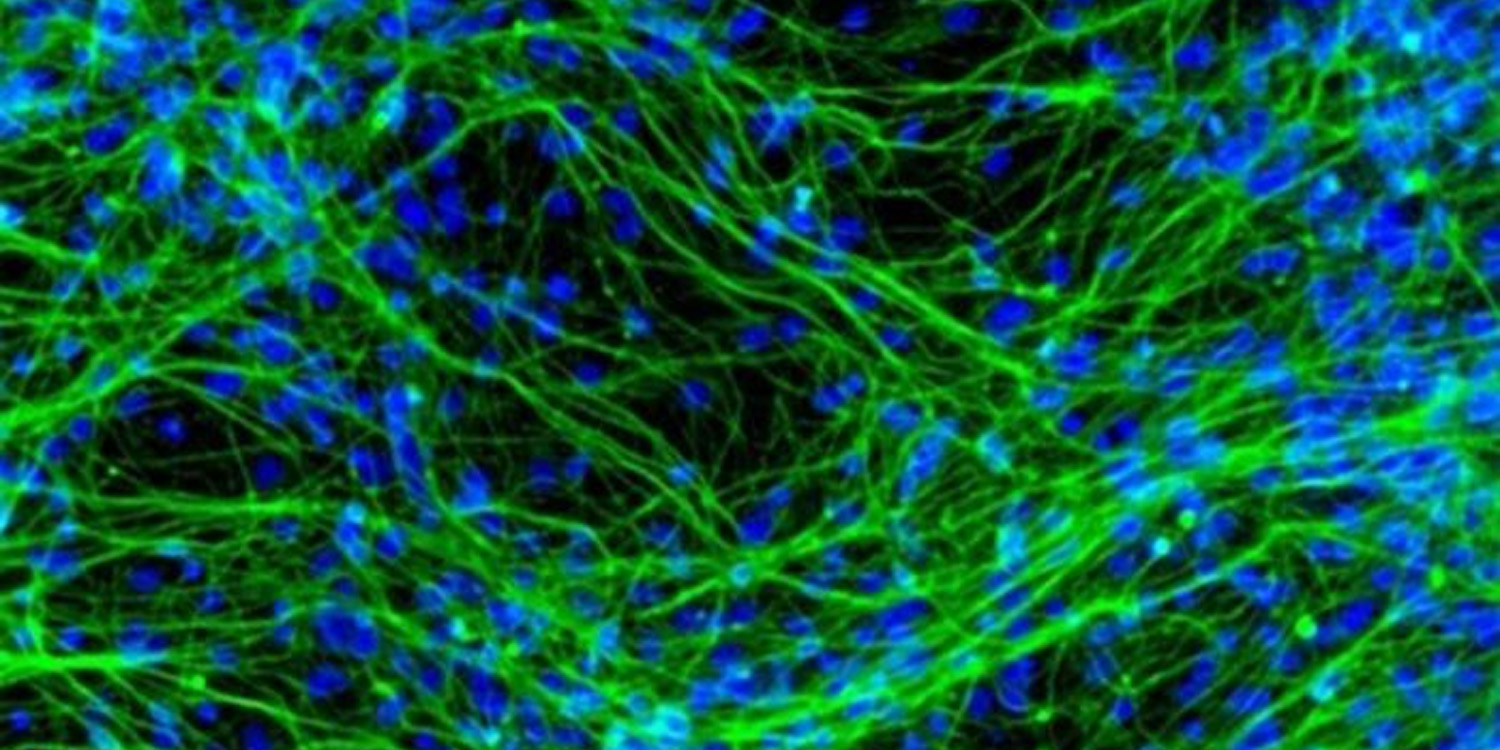
Delta opioid receptors (DOPs) are a type of opioid receptor, one of several receptors activated by the body’s natural opioid peptides as well as by synthetic and plant-derived opioids. These receptors are part of the larger family of G protein-coupled receptors (GPCRs), which play critical roles in transmitting signals from the outside of a cell to its interior. DOPs are predominantly localized in the brain, particularly in areas involved in pain modulation, emotional response, and neuroendocrine regulation.
Despite the known role of DOPs in emotional regulation, no drugs targeting these receptors are available for treating anxiety and depression. This gap in treatment options propelled the research team to explore DOP agonists as potential alternatives. Their focus on KNT-127, a compound that shows promise in animal models for its anxiety-reducing effects without significant side effects, aimed to understand how it achieves these effects at the molecular level.
“There are currently no therapeutic drugs mediated by delta opioid receptors (DOPs). DOPs likely exert anti-depressant and anti-anxiety effects through a mechanism of action different from that of existing psychotropic drugs. DOP agonists may, therefore, be useful for treatment-resistant and intractable mental illnesses which do not respond to existing treatments,” explained study author Akiyoshi Saitoh, a professor at Tokyo University of Science’s Faculty of Pharmaceutical Sciences.
The study’s methodology was anchored in optogenetics. This technique represents a fusion of genetics and optics, allowing scientists to control specific neurons in the brain with light. The researchers specifically targeted a neural pathway from the prelimbic cortex (PL) to the basolateral nucleus of the amygdala (BLA), both critical areas in the brain associated with the regulation of emotions and the development of anxiety.
To begin, the team injected male C57BL/6J mice with a virus carrying the gene for channelrhodopsin-2 (ChR2), a light-sensitive protein, or a control virus, directly into the PL. This setup enabled the neurons in the PL-BLA pathway to respond to light, allowing for precise control over this circuit’s activity.
Following the viral injection, an optic fiber was implanted above the BLA to deliver light pulses, effectively activating the PL-BLA pathway on demand. This sophisticated optogenetic stimulation setup was crucial for investigating how specific activation of this pathway influences anxiety-like behavior in mice.
The researchers then conducted a series of behavioral tests to assess the effects of activating the PL-BLA pathway on anxiety-like and fear-related behaviors. The elevated plus-maze test, a widely used assay in animal anxiety research, was utilized to evaluate innate anxiety-like behavior. This test exploits a mouse’s natural aversion to open, elevated spaces, with increased time spent in open arms indicating reduced anxiety.
Additionally, the open-field test was used to measure anxiety by recording how much time the animals spent in the center of an open arena, with more time in the center suggesting lower anxiety levels. The contextual fear conditioning test was employed to assess learned fear responses, with freezing behavior serving as an indicator of fear.
The findings from these experiments were revealing. Activation of the PL-BLA pathway led to increased anxiety-like behavior, as mice spent significantly less time in the open arms of the elevated plus-maze and the center of the open-field arena, indicating heightened innate anxiety. However, when it came to learned fear responses assessed by the contextual fear conditioning test, there was no significant difference between mice with activated PL-BLA pathways and controls, suggesting that this circuit’s role in anxiety is distinct from its involvement in conditioned fear responses.
Further illuminating the potential therapeutic benefits of targeting this pathway, the administration of KNT-127, a selective DOP agonist, significantly reduced anxiety-like behavior in mice with activated PL-BLA pathways. Mice treated with KNT-127 spent more time in the open arms of the elevated plus-maze and the center of the open-field arena, indicating a decrease in innate anxiety. This effect was specific to the activation of the PL-BLA pathway, as KNT-127 did not significantly alter the behavior of control mice or those subjected to conditioned fear tests.
These findings underscore the pivotal role of the PL-BLA pathway in regulating innate anxiety and demonstrate the potential of DOP agonists, like KNT-127, in alleviating such anxiety through the modulation of this specific brain circuit.
“The brain neural circuits focused on in this study are conserved in humans, and research on human brain imaging has revealed that the PL-BLA region is overactive in patients with depression and anxiety disorders,” Saitoh said. “We are optimistic that suppressing overactivity in this brain region using DOP-targeted therapies can exert significant anxiolytic effects in humans.”
The study, “The delta opioid receptor agonist KNT-127 relieves innate anxiety-like behavior in mice by suppressing transmission from the prelimbic cortex to basolateral amygdala,” was authored by Ayako Kawaminami, Daisuke Yamada, Toshinori Yoshioka, Azumi Hatakeyama, Moeno Nishida, Keita Kajino, Tsuyoshi Saitoh, Hiroshi Nagase, and Akiyoshi Saitoh.