Mrs Stephenie Agbaje and her husband were so madly in love that they did not bother to go for a genotype test before getting married. They believed that their love and companionship would conquer whatever obstacle that would come their way. This was a costly mistake because both of them are carriers of sickle cell trait (AS).
They swirled in their love until the point when Mrs Agbaje got pregnant. She looked forward to a beautiful and fulfilling motherhood with a bouncing baby. But the sad news is that her child had sickle cell anaemia.
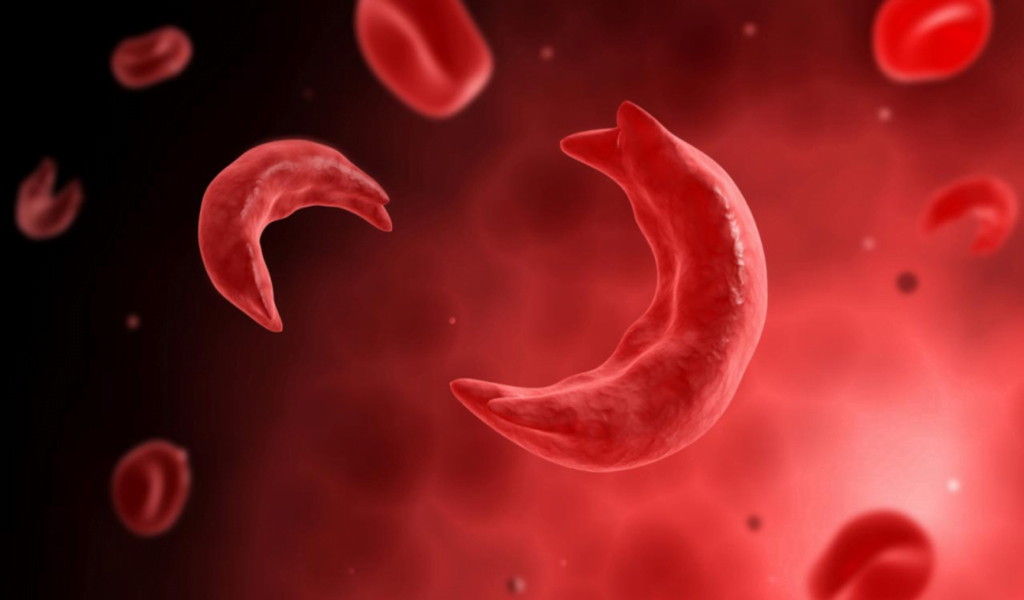
Sickle cell disease (SCD) is a genetic blood disorder characterised by abnormal red blood cells that take on a crescent or sickle shape and these irregularly shaped cells can cause blockages in blood vessels, leading to a variety of health complications.
Over time, individuals with the disease may experience organ damage to the liver, kidneys, lungs, heart, and spleen. And complications from the disorder can also lead to death. The treatment of sickle cell disease primarily focuses on preventing and managing these complications.
According to experts, Nigeria bears the highest burden of SCD globally and is the top sickle cell endemic country in Africa, with an annual infant death toll of about 150,000, representing more than 8 per cent of infant mortality in the country.
“Approximately 50 million people are living with sickle cell disease in the world, with Nigeria being the epicentre and home to about 4-6 million individuals with the disease.
Also each year, around 300,000 newly diagnosed sickle cell children are born worldwide, and at least 100,000 babies in Nigeria die from the disorder, making it the number one sickle-cell endemic country in Africa, as per 2014 statistics from the World Health Organization (WHO)”, said Dr Annette Akinsete, Consultant Public Health Physician and the National Director/Chief executive officer of the Sickle Cell Foundation Nigeria.
Living with sickle cell disease is a huge challenge both for the carrier and his loved ones. Individuals with the condition experience chronic pain, fatigue, and other symptoms that can affect their quality of life.
Hence the news that her child is a sickle cell patient, shattered Mrs. Agbaje and family. It was not what she bargained for in her first pregnancy experience. And from day one, she and her child passed through traumatising experiences.
However, Mrs. Agbaje and her daughter, who is now 23 years old, have lived to tell the story and provide support to other families. And it is in her bid to contribute in the fight against sickle cell that Mrs Agbaje has stepped up to use her personal experience of raising such a child with severe health difficulties and regret, to help other families who are trapped in the same boat.
She launched an organisation, Marvel Sickle Cell Foundation, that is now in the forefront of advocacy for over 17 years, educating people on everything about this disease.
Narrating her ordeal, Mrs. Agbaje in a chat with DAILY POST said that the reality of her situation first dawned on her when the pregnancy test came out positive.
“I did a lot of fasting and prayer, expecting a miracle, but six weeks after my daughter was born, a blood test confirmed her haemoglobin to be SS. I was completely devastated. I felt like heaven had forsaken me. Within her first year, I found out that her condition was serious.
“Doctors said my child’s major complication was acute chest syndrome, which occurred during a crisis attack. And whenever it started, she would feel like her chest would divide into two.
“Whenever she goes through those attacks. I watch my child helplessly as she screams out in pain. I will cry and wish that I could help her bear some of her agonies but I can’t and on those times, I weep and ask God why my little girl has to go through so much agony,” Mrs. Agbaje said.
After all those trauma 23 years ago, Mrs. Agbaje, and her daughter, Marvellous, have come out stronger and are now ‘Sickle Cell Warriors.
They have decided to use their story to inspire courage, resilience, and hope in families battling the disease.
“My daughter is a survivor. She is a graduate of criminology from the National Open University, Akure campus. It’s been a bittersweet roller-coaster of emotions,” she reminisced.
“The peak of her crisis was her early and formative years when we were always in and out of the hospital, with bills to pay and issues here and there.
“The most recent challenge we had was when she couldn’t attend her convocation ceremony earlier this year because she was in hospital when her mates were jubilating on their awarded degree,” she added.
Indeed, the condition of Sickle cell patients in Nigeria is pathetic. This is not only because of their limited access to healthcare and treatment options but also of the social stigmatisation and discrimination they are made to suffer. According to Mrs Agbaje, she and her daughter experienced firsthand stigmatisation from family and friends.
And this is because society thinks that the sickle cell ailment is foisted on people by an evil force or via spiritual curses.
“My family deserted me and told me that they have never had a child with such health challenges in their lineage. Even someone once asked me why I was wasting my time and money on a child who would die.
“But I told her that everyone’s life is in God’s hands. Moreover, even healthy people die every day. So why should anyone try to taunt me by saying my daughter would die?
“Most African parents believe that sickle cell carriers are witches, or evil children sent to torment their families. But we shall continue to educate people to let them know the disease is not infectious. They are not ‘Abiku’ or ‘Ogbanje’. They are just victims of other people’s ignorance.
“I heard about a man who chased his wife and child away. I have also seen some fathers who accused their wives of getting such children from water spirits. A mother once asked me, ‘Why does my child fall ill just after I have collected my monthly salary?’
“It hurts to work throughout the month and use the salary to buy drugs for a sick child. The blood of a sickle cell carrier breaks down every 28 days, unlike other genotypes that break down every 30 days. That is why sickle cell patients always fall sick towards the end of the month.
“We can only keep educating them. Sensitization programmes are important to change the narrative. There are no evil forces anywhere. Their problem is purely science and genetics so we should pay more attention to our biological compositions like genotype so we can enjoy a healthy living,” she said.
Last Monday was World Sickle Cell Awareness Day, a day observed every year to raise awareness about sickle cell disease (SCD) and its impact on individuals, families and communities worldwide.
And speaking on the theme, ‘Building and strengthening global sickle cell communities, formalising newborn screening and knowing your sickle cell disease status’, Mrs. Agbaje urged Nigerians to recognise the first step to understanding the genotype in infants and adults in fighting sickle cell disease.
“Every Nigerian must be aware that they deserve to have a happy home and healthy children”, she said.
“No child should live in pain and health restrictions for the rest of her life. They should care because it is their civic responsibility to consider society in whatever decision they take.
“After all, the moment a child is born he/she becomes a member of the larger society and a responsibility of the society whether we like it or not.
“The society deserves a sickle cell-free society. Gone are those days when our parents got married without performing the necessary medical screening. I would advise every couple to check their genotype before getting married.
“Go to l hospitals and be sure that both of you are compatible. Many marriages have broken up today because of this issue, and many children are suffering because of the mistakes of their parents.
“So don’t take that risk. Also, if you have a child or know anyone suffering from sickle cell disease, don’t stigmatise them. While they are still alive, please give them a reason to be happy”, Mrs Agbaje added.
Another expert, Ibrahim Rukayat, from the Center of Excellence for Sickle Cell Disease Research & Training (CESRTA), University of Abuja, harped on the need for more newborn screening to help decipher their genotype.
According to her, early identification of the baby’s genotype through newborn screening allows for prompt diagnosis and management of the condition.
This, she said, involves hospital treatment, as well as counselling and health education to promote the baby’s survival and well-being.
She said babies born with the disease could develop complications and die within three to six months of birth.
“For instance, out of the 136 babies that we have identified, seven are dead already. So based on the quantity of the sickle cell genotype in their blood, humans differ from each other – the rate some people may respond to malaria is quite different from others – so early management is important,” she said.










